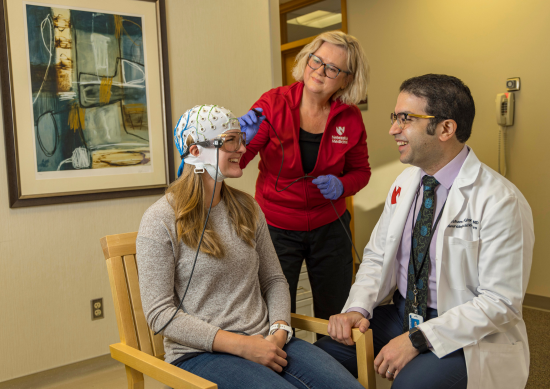
When evaluating patients with epilepsy for surgery, timing and accuracy are critical. The MEG Center at Nebraska Medical Center provides referring physicians with a unique combination of cutting-edge technology, expert analysis and expedited service that sets it apart from other regional centers.
What sets the MEG Center apart
The center is one of only 24 facilities in the U.S. using magnetoencephalography (MEG) to noninvasively evaluate patients for epilepsy surgery.
“Not every hospital, or even every state, has MEG,” explains Valentina Gumenyuk, PhD, core director of the MEG Center, which serves patients from across the region.
Rapid turnaround: The most significant advantage for referring physicians is speed. “We generate clinical reports within a couple of days, where other centers may take a month,” Dr. Gumenyuk says.
Urgent access: For patients who need expedited evaluation, the center offers quick scheduling. Referring physicians can select “urgent” on the referral form, and the patient will be scheduled ahead of routine cases.
Maximizing diagnostic yield
A critical differentiator of the MEG Center is its commitment to obtaining actionable results for every patient. At other centers, patients may be reported as “not cooperative” or unable to sleep, resulting in no diagnostic information despite the significant cost and preparation involved.
The Nebraska Medicine team takes a different approach through meticulous pre-test preparation, including:
- Detailed sleep consultations.
- Customized strategies combining sleep deprivation and sleep aids when appropriate.
- Proactive behavioral preparation for pediatric patients or those with previous negative testing experiences.
For patients with electrode intolerance, MEG-only recordings can provide diagnostic quality results without the EEG component.
“We try to minimize negative results as much as possible to ensure every patient has a result from our study,” Dr. Gumenyuk says. This commitment ensures that referring physicians receive the critical information they need.
The MEG advantage: More than seizure localization
Magnetoencephalography offers distinct advantages over traditional EEG. As medical director Hesham Ghonim, MD, explains, “The highly sensitive sensors inside MEG detect magnetic fields that pass unobstructed through those layers from the brain to the outside,” unlike EEG signals that must pass through scalp, skull and fluids.
MEG serves two critical functions in pre-surgical evaluation:
Epileptic focus localization: The technology identifies where seizure activity originates with millimeter-level precision. “Many studies have shown that resection of brain regions with MEG activity translates into a higher chance of seizure freedom,” Dr. Ghonim says. However, MEG can also be a game-changer by revealing that surgery isn’t feasible. “MEG may show surgery is not possible because of activity happening in different regions,” Dr. Gumenyuk explains.
Functional brain mapping: Perhaps equally important, MEG maps critical brain regions – motor cortex, language areas, auditory and visual processing centers – with exceptional temporal and spatial resolution. “We map the brain quite thoroughly,” says Dr. Gumenyuk. “That information is very valuable for the surgeon making a decision.”
Comprehensive patient care across all ages
The MEG Center serves patients from newborns to 85-year-old adults, with approximately 40% pediatric and 60% adult cases. The team has developed specialized protocols to maximize cooperation and minimize negative results.
Sleep optimization: Since 95% of diagnostic data comes from sleep recordings, the center works closely with patients and families on sleep preparation.
Pediatric expertise: For children, especially those with sensory challenges or anxiety about medical procedures, the team takes extra measures. Parents can remain in the MEG room during recording, providing comfort and confirming seizure activity if it occurs.
Flexible protocols: For patients who cannot tolerate EEG electrodes due to sensory sensitivity, MEG-only recordings are possible. The MEG helmet design keeps the face open and allows for a comfortable sleep position.
Improved precision: For patients with craniotomies, skull abnormalities or infants with undeveloped skulls, MEG’s magnetic signal provides superior accuracy compared to EEG’s electrical signal.
Real-world impact: A clinical success story
The center’s capabilities were showcased in a published case of a 14-year-old with Rasmussen encephalitis. The child had deteriorated from normal development to experiencing 50 seizures daily, loss of speech and mobility and feeding tube dependence.
MEG mapping revealed that despite being right-handed, his language function had migrated – critical information for surgical planning.
“We showed the surgeon that language had migrated to his right hemisphere,” Dr. Gumenyuk says. This finding enabled safe left hemispherotomy. One-year post-surgery, the patient is seizure-free, speaking and walking normally.
Expert team, advanced technology
The MEG Center utilizes the MEGIN TRIUX™ neo, the most advanced MEG technology available. The equipment compensates for head movement and can study patients with metal implants or dentures.
Equally important is the team’s expertise. Leading researchers, with 20 years of experience in the MEG field, work collaboratively on every case.
When to refer
Timely referral is crucial. “It’s been shown that the quicker drug-resistant epilepsy patients are evaluated for surgery, the better their outcome,” Dr. Ghonim notes.
Consider MEG evaluation for patients with:
- Drug-resistant epilepsy being considered for surgery.
- Need for precise localization of epileptic focus.
- Seizures near eloquent cortex requiring functional mapping.
- Complex or unclear cases where surgery feasibility is uncertain.
- Urgent surgical evaluation needs.
Because MEG is often performed once in a patient’s lifetime as part of comprehensive pre-surgical workup, the quality and timeliness of results are paramount. The Nebraska Medicine MEG Center delivers both.
To refer a patient or for urgent cases, call 402.552.9660.