What is gastric bypass surgery, and who is eligible?
For many people, losing weight isn’t a “one-size-fits-all” and not always as simple as eating less and exercising more. It can feel like an uphill battle due to genetics, metabolism or potential mental health challenges. That’s why gastric bypass surgery can be a life-changing treatment for people whose health is at risk. It can help people reclaim their health, mobility and overall quality of life, especially when other options haven’t worked.
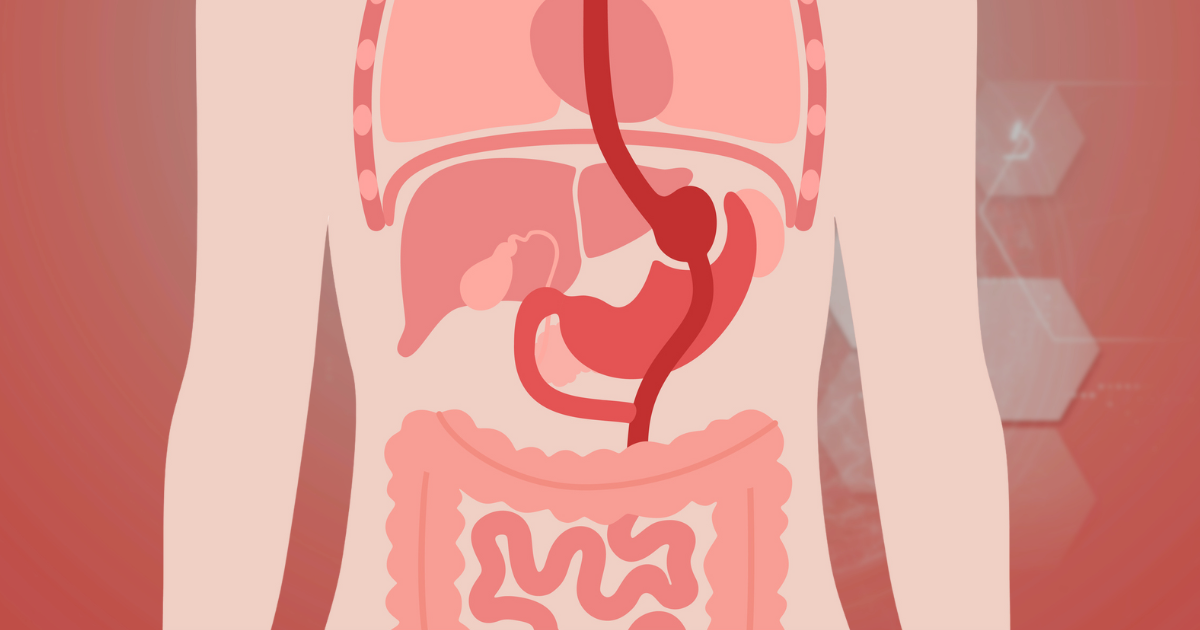
Gastric bypass surgery, also called Roux-en-Y gastric bypass, is a bariatric surgery that can change how your stomach and small intestine handle food.
“A small gastric pouch is created at the top of the stomach, which becomes the new stomach and limits how much food you can eat at one time,” says Nebraska Medicine bariatric surgeon Anthony Murante, MD. “The small pouch is connected directly to a lower section of the small intestine.”
This means food bypasses most of the stomach and the first part of the intestine. As a result, you take in fewer calories and lose weight.
Why it’s done
“Gastric bypass is recommended for those with severe obesity, usually with a BMI of 40 or higher,” says Dr. Murante. “These patients may have serious health problems like sleep apnea, hypertension or type 2 diabetes.”
The surgery can also help improve other health problems, such as high blood pressure, heart disease, joint problems, limited mobility and fatty liver disease. Carrying excess weight and lymphedemas from extreme swelling and fluid buildup can be painful and make it difficult to do everyday chores, walking or playing with kids.
Sometimes diet, exercise or weight-loss medications aren’t enough. For those patients, gastric bypass can be a tool to help regain their quality of life.
Gastric bypass vs. gastric sleeve
“With gastric sleeve, or sleeve gastrectomy, about 80% of the stomach is removed and a ‘sleeve’ is left behind,” says Dr. Murante. “Food passes through normally without rerouting the intestines.”
Like gastric bypass, the gastric sleeve results in a smaller appetite. The sleeve is a good choice for people who want a less complex weight-loss surgery or may be at a higher risk during surgery.
Who qualifies for bariatric surgery?
If you’ve tried everything and still struggle with obesity, surgery may be a life-changing next step. Candidates often have:
- A high BMI of over 40.
- A waist size between 35 and 40 inches.
- Weight-related health issues.
- A strong commitment to a lifestyle change.
Gastric bypass candidates cannot have active drug or alcohol abuse. Pregnancy, liver disease, inoperable cancers and medically reversible obesity may also disqualify someone from surgery.
Before the surgery
“We have patients go through comprehensive medical and psychological evaluations to ensure long-term success and safety,” says Dr. Murante.
Medical tests may include checking liver and kidney functions, thyroid function, blood sugar levels, sleep studies and nutrient deficiencies. X-rays and EKGs assess heart and lung health before surgery.
A registered dietician will review your eating habits and teach you about portion sizes, nutrition and protein needs. You’ll also have a mental health screening to make sure you’re emotionally ready and to treat any potential depression, eating disorders or substance abuse.
“We want to start seeing lifestyle adjustments for patients,” says Dr. Murante. “That can mean exercising, making diet changes and identifying support systems for after surgery.”
Life after surgery
Most patients recover within 3 to 6 weeks and can return to work and light activity. The bulk of weight loss happens over the next year, where patients are watched closely to ensure they’re hitting weight loss and nutritional goals.
“At about 6 weeks is when we start formally tracking the weight,” says Dr. Murante. “About every 3 months, we’re monitoring weight and running vitamin panels. This helps reassure patients that they’re on track for their goals.”
After surgery, the diet progresses in careful stages to help the stomach heal and prevent complications. It’s important to stay hydrated to prevent nausea.
“The post-surgery diet goes through several iterations,” says Dr. Murante. “For the first 6 weeks, we teach patients to eat smaller portions slowly. They start with a liquid diet and add in protein, increasing the food consistencies from puréed to soft. We tell patients to build their diet outward; start with a lean protein, add in non-starchy vegetables, and low carbohydrates. There aren’t any other stipulations, but we do educate on which foods to stay away from.”
For most patients, gastric bypass surgery helps regain health, confidence and happiness in life. Patients may feel like they’re living for the first time and enjoying things they once couldn’t.
“Patients see weight come off, and they’re able to be more mobile and confident,” says Dr. Murante. “This helps with their activity levels and reduces difficulties at the gym. We see quick improvements in medical conditions. Patients with diabetes, for instance, may come off diabetes medication quickly.
Recovery after gastric bypass surgery isn’t just physical. Emotional changes are common too, when food is linked to comfort and a sense of safety. Therapy and support groups can make a difference post-surgery.





