[Q&A] The latest on omicron symptoms, at-home COVID-19 tests and treatment options
In this video, watch infectious diseases experts Mark Rupp, MD, and Armando De Alba Rosales, MD, MPH, answer your questions about the omicron variant.
What we know about omicron changes quickly, so check credible information sources for the latest.
Jump to a specific question:
- [0:48] We knew that variants were going to change and that this was going to evolve. What makes the omicron variant so different and so concerning?
- [4:27] Why are cloth masks not as effective against omicron? What do we need to consider if we're going out in public?
- [8:13] What COVID-19 treatments work against omicron? What's the availability like?
- [10:53] Since this variant is less severe, some people may think it's best to just get infected to get immunity. Is that a fair thing to say or is it best not to get COVID-19 at all? Will basically everyone get the variant at this point?
- [14:48] Are omicron symptoms different? Is the loss of taste and smell still happening with omicron? What are the signs of COVID in babies?
- [16:39] Can current COVID-19 tests detect omicron? Are at-home tests dependable?
- [18:52] What are the guidelines for isolating if there's a case within my home? If one family member tests positive, does that mean everyone stays home?
- [24:02] What if I get flu and omicron at the same time?
- [25:29] How can I take care of myself at home with COVID-19? What can I do to manage symptoms?
- [28:50] How long is a disposable procedure mask good for?
- [29:38] Do we need to clean surfaces or worry about surface transmission with omicron?
- [30:24] Closing thoughts about omicron and COVID-19
We knew that variants were going to change and that this was going to evolve. What makes the omicron variant so different and so concerning?
Dr. Mark Rupp: "The emergence of variants is something that we have expected all along. And we've seen multiple variants. People had trouble keeping up with variants at first because they had these funky numbers and then they started using the Greek alphabet. I hope we don't run out of Greek alphabet letters, but we could.
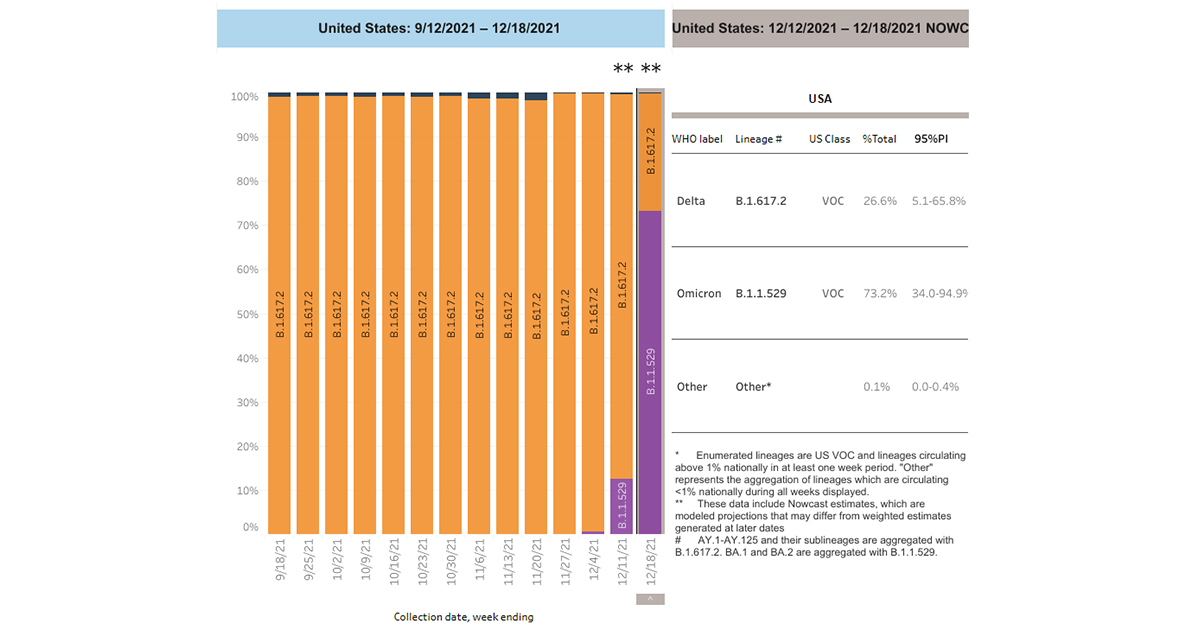
"The omicron variant was first described down in South Africa late in November and it has just exploded. It really is much more transmissible than other variants and that became painfully obvious within days of its first description. It was being described more widely in South Africa, more widely in the region and then within just weeks, it was worldwide. We've seen the same thing here in the United States where its doubling time seems to be about two days or so. This is almost a logarithmic, sort of exponential spread that we are seeing in the U.S.
"Clearly it is the predominant strain here in Nebraska. It has mutations in a number of areas that predict its characteristics and its behavior so it's more transmissible. It has lots of mutations in what we call the spike protein, which allows it to interact with human cells. We think this is why it is able to bind more avidly or transmit more easily between humans. There are also some interesting characteristics that were described where it seems to proliferate more in the upper airways and not so much in the lower airways. So this might explain this phenomenon we're seeing of potentially more mild disease. But I don't want to give people the wrong idea. When we look at it on a population basis, this is very, very serious. The sheer numbers of cases that we see coming to the community will predict for a greater number overall of hospitalizations – even though percentage-wise it may be less requirement of hospitalizations. The vaccine – particularly if you have been boosted – appears to protect against severe disease, hospitalization and deaths even with the omicron variant. So it's really important for people to do those nonpharmacological interventions."
Dr. Armando De Alba: "It is also important that we take into consideration that our kids are being impacted by omicron, so we need to protect them. A lot of kids are not qualified to receive the vaccine – especially those who are younger than five years. We need to take this seriously and follow the preventive methods in order to protect them. We see in our hospitals that kids are getting sick with this new variant and hospitalizations are increasing significantly among this population."
Why are cloth masks not as effective against omicron? What do we need to consider if we're going out in public?
Dr. De Alba: "In general, masking has many functions. One is to prevent it in those infected, it prevents passing the virus to other people. Second, it prevents the other person from inhaling the virus or getting infected with the virus. In these times with omicron, which is highly contagious, we know SARS-CoV-2 is airborne and the quality of mask we use really matters. That's why we are now recommending going with a higher grade of protection: surgical masks, N95 where possible or KN95. When we look at the studies and compare them with cloth masks or bandanas, those cloth masks offer very little protection compared to the surgical mask and the N95. So these are general principles why now we're recommending these kinds of masks and it is important that we look for those masks also that cover the face and also protect areas where there might be some holes."
Dr. Rupp: "Like we've seen with all of the previous variants of COVID-19, people are most infectious just before they get ill if they're going to develop symptoms and when they develop symptoms, they can be very mild or have asymptomatic illness and be shedding large amounts of virus.
"I think that some people have this idea that I'm going to put on a mask if I start having cold symptoms (like when I start to cough) so I'll protect everybody then. Or, if I see somebody who's got a runny nose, I'll put my mask on and protect myself. That just isn't going to work with this variant. It's very transmissible. The incubation period appears to be shorter. So it's going from person to person to person very, very quickly.
"It's just really important for us to do these nonpharmacologic interventions, as Dr. De Alba said. Get the best-fitting, best-constructed respiratory protection that you can have. Multiple layers, well-constructed, fitting tightly to the face is really what we're looking for, as well as people showing good judgment when they are out in public.
"Avoid those high-risk settings, particularly here over the next few weeks. I know people are really tired of hearing this, but this is really important right now at this juncture for the next few weeks. Let's really buckle down and start to show some good judgment. So crowding into your favorite restaurant or bar or going to your favorite sports facility – probably not a good thing to do right now. Give it a few weeks and then hopefully we'll see this peak come down quickly and then maybe people will be able to lighten up just a little bit."
What COVID-19 treatments work against omicron? What's the availability like?
Dr. Rupp: "This is a very important thing for people to understand. Even though they may have been reading about some of these new medications that are coming out, that these are in such desperately short supply that for the most part, they're not going to be available to people to rescue them if they get ill.
"Some of the monoclonal antibodies that people have heard about, that have been developed in the last year or year and a half, are not effective against omicron. The virus has shifted and those monoclonals just don't interact with the virus any longer – they're not going to be effective.
There's one monoclonal called sotrovimab that's effective but we have very, very few doses of that. We're only able to give here at the medical center about four to five people per day that infusion and we have dozens of folks who qualify for it. We're giving it only to those people with the highest risk of progression of disease.
"There's also another monoclonal that has a very long-lasting effect called evusheld, which is a combination of some of these monoclonals, but few doses are available. In our system, we estimate that we have somewhere around 9,000 to 10,000 patients that would qualify for it but we are only able to give about 50 of those doses per day to try to prevent illness. This isn't a treatment, it's prevention.
"People have heard about some of these oral medications that have come out like paxlovid and molnupiravir. There are very, very few doses. We are just not able to treat most people.
"The last one that I would mention is remdesivir, which is effective in preventing progression of disease but has to be given intravenously over three days. Logistically it's really, really difficult as you can imagine, to get somebody into an infusion center for three days in a row to try to prevent the progression of disease. And we are reserving this for the most highest risk people. So the best thing to do is prevent the disease in the first place by getting your booster. And second, don't put yourself in harm's way."
Since this variant is less severe, some people may think it's best to just get infected to get immunity. Is that a fair thing to say or is it best not to get COVID-19 at all? Will basically everyone get the variant at this point?
Dr. De Alba: "We cannot depend on herd immunity, that's actually inhumane. If we depend on herd immunity, a lot of people will die. We know omicron is highly contagious. The more people get infected, the more people will die, according to the math and projections. And we will see the health care system be impacted.
"When we talk about severity, I want people to see the broader perspective. What do we mean by severity? If we look at it from the health care system perspective, this is very, very bad and we haven't experienced something like omicron. So this could be very catastrophic and that's what we are trying to prevent.
"The good news is we have preventive measures that are efficient and proven to be helpful to reduce the spread of the virus. And that's what we are striving for. We also want to promote the preventive measures – which is vaccination, masks, social distancing – because we know they are efficient and we want to help the health care system. This is not just about the biological process, it's also about the social determinants of health we need to keep in consideration we talk about this pandemic."
Dr. Rupp: "Herd immunity does have some intuitable appeal to it, right? So if everybody had a very mild disease – just a little bit of a cold and then they were immune to the illness – great, let's do it. But the problem is there are two problems with that. Number one, you're not guaranteed to have a mild illness particularly if you have risk factors for more severe disease. And so we are seeing people get severely ill, come into the hospital and undoubtedly the death rate will start to rise throughout the country.
"The second point is we really don't know what the natural disease-induced immunity is going to be with omicron. With previous variants, when people had more mild disease, it sometimes equated with less of a robust immunologic response and not being left with less protective immunity. We have also seen with disease-induced immunity that it can be very spotty. Some people can get a great robust immune response and others very little immune response. The best way – the most standardized and best approach to this is to get the vaccine – make sure that you have a robust response that's very predictive, as opposed to the more spotty disease-induced immunity that may not be long lasting.
"I would plead for people not to have the chickenpox party like we used to have as kids when we wanted to get everybody in the family immune to chickenpox. That's a bad approach when we have such a better way of approaching this which is getting the vaccine."
Are omicron symptoms different? Is the loss of taste and smell still happening with omicron? What are the signs of COVID in babies?
Dr. Rupp: "It's pretty much the same as what we've seen with the other variants. It's a little bit more mild, less of the lower respiratory tract symptoms of shortness of breath and then not being able to get enough oxygen with more of a multi-inflammatory response or sepsis kind of response. So we're seeing less of that, although there are some cases of it. And certainly the other symptoms of fever, sore throat, headache, nasal congestion, cough – all of those we continue to see, maybe a little bit less of the reduced taste and smell."
Dr. De Alba: "I would also like to add when it comes down to kids or particularly babies – check if they have difficulty breathing. For example, look at the chest for signs of difficulty breathing. Another thing to look at is their diaper. If the diapers are dry, that raises a flag. So we are seeing these specific elements with babies, so keep an eye on the health of your children."
Can current COVID-19 tests detect omicron? Are at-home tests dependable?
Dr. Rupp: "I know people feel demoralized by this recent variant. I would just like to emphasize that we are in a better spot than we were two years ago, quite clearly. So we have an effective vaccine, we have some medications that are effective. We know so much more about this illness and how it spreads. So we are in a better place so don't hey demoralize, don't lose hope, don't be fatalistic that this is going to completely derail us.
"However, having said that, testing has been kind of a sore point. In the very, very early days of the pandemic, we did build up a more robust testing system, but then as we had the vaccine come in, we really dismantled that. So for example, here in Nebraska, we don't really have as ready access to testing as we need. In addition, there are differences between the tests and without getting into too great of detail, the rapid antigen tests appear to be less sensitive, particularly in the early phase of the disease. So they may be a little less reliable with omicron. The PCR continues to be a very sensitive test, but it's a little harder to get access to.
"The other problem I would point out is many of the home rapid antigen tests are really completely off the radar for public health. We are not able to track those and figure out where the patterns of disease are. There are a lot of issues with testing that we continue to work on. And I don't say this in any disparaging way to my colleagues in the laboratory. Those guys have been working day and night for two years. I have the utmost respect and admiration for them."
What are the guidelines for isolating if there's a case within my home? If one family member tests positive, does that mean everyone stays home?
Dr. De Alba: "It's important to have open communication with those whom with you interact. Get to know the vaccination status of those whom you socialize with so if there is a positive case there can be contact tracing. So if someone comes with symptoms, that person should be isolated until it's shown that person isn't positive. The recommendation will be to get a test – a PCR continues to be the gold standard. But if that isn't possible and you know that you were interacting with someone who was positive and diagnosed with COVID-19 and you start to develop symptoms – you should start to follow recommendations for isolation. You should contact your health department if you don't have access to a clinic or a hospital. Then follow their instructions because there will be a process for contact tracing and they will guide you when you can return to normal activities. CDC recommends isolation for five days and then testing. If the test is positive they should isolate for another five days."
Dr. Rupp: "I wish we had fast, accurate, readily available cheap testing for everybody but it's not reality. So I think people are responding to that by sort of picking and choosing when they get tested. I understand that and again I would plead with folks that if they are symptomatic, to take themselves out of circulation and put themselves into isolation. If they don't have a diagnosis, it's probably good to assume they have it because it's just so prevalent in the community. And so the best practice is, like Dr. De Alba said, put yourself in isolation for 10 days before you come back out. If you get that test at five days and it's negative, and if you have to go back to work, please do so wearing a mask."
Dr. De Alba: "If you see that your symptoms aren't improving and are getting worse, seek medical attention. Some people have access to pulse oximeters and they have learned how to use an oximeter. If you have access to a pulse oximeter and check your result and it's below 90, seek medical attention because that's when you actually need to receive other complementary things that we can offer in the hospital. It's a common question in the community, particularly where some don't have access to a physician."
Dr. Rupp: "The other issue is there are other respiratory viruses circulating, as well, including influenza. We have some good medications for influenza so it does behoove people to get a test and figure out which virus they're infected with because it's different how we manage those."
What if I get flu and omicron at the same time?
Dr. Rupp: "Last year we had a nonexistent flu season. Maybe partly due to the fact that people were putting these precautions into place. Also, a lot was due to viral dynamics and how it interacts with the human population. We don't fully understand those interactions at this point.
"We're not going get that lucky this year and we're already seeing H3N2 influenza circulating in the community. It can be a severe disease as well. You can have both of them together and data would suggest if you have a coinfection that your outcomes are worse. That doesn't really come as that much of a surprise. There is some information out there, believe it or not, that getting a flu vaccine actually has you do better with COVID-19 and so there may be some immunologic interactions there that aren't fully understood. But the data is fairly strong that getting the flu vaccine may actually help you cope with COVID as well. That's another good reason to get the flu vaccine. I already gave you the reasons to get the COVID vaccine."
How can I take care of myself at home with COVID-19? What can I do to manage symptoms?
Dr. De Alba: "Stay hydrated, have good dietary habits, vegetables and fruit, get rest and isolate. I know it's tiring, I know it's challenging to stay at home in four walls, but it's one of the most effective ways to protect others, particularly those who surround you. A large segment of our population also lives in a large household so a lot of the time you have only one bathroom and they have to share with other members. It's important that when you have to use common spaces, wear a mask to protect those around you and who you love."
Dr. Rupp: "I completely agree to do your self-isolation, protecting your other family members. I would say taking a little bit of acetaminophen (otherwise known as Tylenol), ibuprofen (otherwise known as Motrin) or something like that is perfectly acceptable to help with the aches and pains and the headache and the fever.
"If you are at high-risk for disease progression: you're elderly, you have underlying cardio-respiratory disease, immunosuppressive disorders, you've had an organ transplant, you're getting cancer chemotherapy, you really do need to plug in with your medical professional. There are some things we can offer, as we've already talked about, to try to prevent the progression of the disease and we need to keep a close eye on you. So those are the people we're most concerned about.
"Otherwise, if you're healthy, you're more than likely going to be able to tough this out at home and we really don't want you to be coming to the emergency department unless it's really an emergency. So if you're doing those things your grandmother told you – rest, fluids, a little bit of Tylenol, and you seem to be doing OK – that's your best bet is just kind of tough it out at home."
Dr. De Alba: "I keep bringing the focus of taking care of the children. We understand that we cannot leave the children in four walls so this is the message: get vaccinated, get your booster because you can be the person who could be the caregiver if your kid needs it. So in that situation, one of the parents can be the caregiver for the kids, take care of your child. So again, it's important that we think also how we can protect the people around us."
How long is a disposable procedure mask good for?
Dr. Rupp: "The best respiratory protection is going to be well constructed and fit tightly to the face. So the procedure masks do fairly well, and if you put some other kind of cloth covering to hold it to your face, it actually functions at a higher level. If you can get your hands on the KN95 – it's even a higher level of protection – it's an important time to do the best protection. When those masks start to get moist, when they get soiled or they start to tear, clearly you want to change out and use a new one."
Do we need to clean surfaces or worry about surface transmission with omicron?
Dr. Rupp: "It's a respiratory disease and it spreads via respiratory droplets. There can be some transmission on surfaces but that's not where the emphasis needs to be. It needs to be on source control, keeping secretions contained, and wearing your own mask to protect yourself. Those are the most important things. Obviously, good hand hygiene, not touching your face, those are the things that can help prevent the spread."
Closing thoughts about omicron and COVID-19
Dr. De Alba: "Even though we are here speaking on behalf of the institution from Nebraska Medicine and UNMC, the message is that combating the COVID pandemic does not start in the hospital or in the clinics. That fight starts in the community. The fight starts within our families, so everybody here plays an important role to end this pandemic. And to end this pandemic, we all need to be onboard regardless of race, nationalities and any other backgrounds."
Dr. Rupp: "I think this is a time when we need to pull together as a community with a unity of purpose. It pains me so deeply to see these issues become politicized and become something that tears us apart. This is a time when we need to come together as a community to protect one another and to do the right thing. So please knuckle down here for a few weeks. Help us get through this. The hospitals are stressed – they are really just teetering on the edge at this point. We need everyone to do what they can to prevent the spread in the community right now."




