7 tips for safe antibiotic use

No one likes to be ill. And it can be even harder seeing your child get sick. You reach for aspirin, ibuprofen, decongestant or cough syrup – anything that might ease the symptoms. And when those don’t do the trick, you may find yourself at your family doctor’s office hoping for a pill or antibiotic that will have your child feeling better again.
It is this common expectation as well as the overuse and misuse of antibiotics over the years that has led to one of today’s most pressing health care problems – antibiotic resistance.
We got you covered. Call 800.922.0000 to schedule an appointment with one of our primary care doctors.
“Unfortunately, there’s a perception that there’s an easy fix to most illnesses,” says Sarah Howard, MD, a Clarkson Family Medicine physician at Old Market Health Center. “But antibiotics do not work for many common illnesses like the cold or flu. Proper antibiotic use and understanding their limitations is a responsibility that we all must play a role in, from doctors and hospitals to consumers.”
Why don’t antibiotics help fight the common cold or flu, you ask?
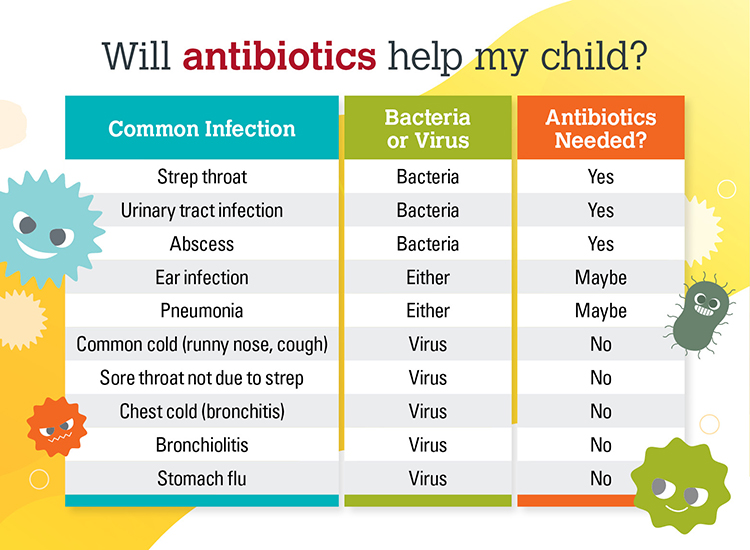
Antibiotics work by fighting infections caused by bacteria. They can either kill the bacteria or make it harder for the bacteria to grow and multiply. When we misuse or overuse antibiotics, the bacteria can change and develop new structures that make them resistant to our antibiotics.
Illnesses like the common cold, flu, most sore throats and ear infections are typically caused by viral infections that are not affected by antibiotics. When we prescribe antibiotics for viruses, it can promote antibiotic resistance. Improper use can also cause adverse side effects like diarrheal illnesses and allergic reactions that can be life threatening.
“Inappropriate use of antibiotics is typically more common with upper respiratory infections, which can sometimes be difficult to diagnose accurately,” says Dr. Howard. “If you have been battling an upper respiratory infection, occasionally it can develop into a bacterial infection so your doctor may decide to try an antibiotic. In addition, when a patient comes to the office and is asking for an antibiotic because they are feeling so badly, it can sometimes be difficult to say no.”
Antibiotic resistance is a real problem that can sometimes lead to death
Antibiotic resistant bacteria can cause illnesses that can no longer be treated and may become life threatening. Methicillin resistant Staphylococcus aureus (MRSA) infection is one of those. MRSA is a type of staph infection often associated with surgeries and hospital infections. Another form of MRSA is spread by skin-to-skin contact and is more common among athletes and child care workers.
An ear infection is an additional infection that is typically virally related that was often overtreated with the antibiotic amoxicillin in years past. As a result, some bacteria are now resistant to this antibiotic.
In an effort to improve the proper use of antibiotics, Clarkson Family Medicine is one of many Nebraska Medicine primary care clinics participating in a year long antimicrobial stewardship program sponsored by the Agency for Healthcare Research and Quality (AHRQ), Johns Hopkins University and the National Opinion Research Center (NORC).
“The goal of this program is to ensure we are prescribing the right antibiotic for the right diagnosis, to the right patient, for the right duration,” says Dr. Howard, who is helping head the program at Clarkson Family Medicine. “We want to improve our role in prescribing antibiotics appropriately and at the same time, educate our patients so they can become responsible users of antibiotics as well.”
Our doctors recommend these 7 tips to help you become a more responsible user of antibiotics:
- Do not demand an antibiotic when you come to see your doctor.
- Take your antibiotics as prescribed and use all pills even if you are feeling better. When you stop taking the pills before you have used them all, there’s a likely chance that all of the bacteria have not been killed and the remaining bacteria will become stronger and replicate new bacteria that will be more resistant to the antibiotic next time around.
- There should not be leftovers, and if for some reason there are, do not save them to take at another time.
- Never share your antibiotics with someone else.
- Always take antibiotics with food to prevent stomach upset.
- If the antibiotic is making you feel worse, talk to your doctor about your symptoms. You may need a different antibiotic or something that will help with the side effects.
- Diarrhea is a common side effect of antibiotics. As a preventive measure, you can take an over-the-counter probiotic to help reduce diarrhea symptoms.



