The heart of cryptogenic strokes: Diagnosing strokes when the cause is unknown

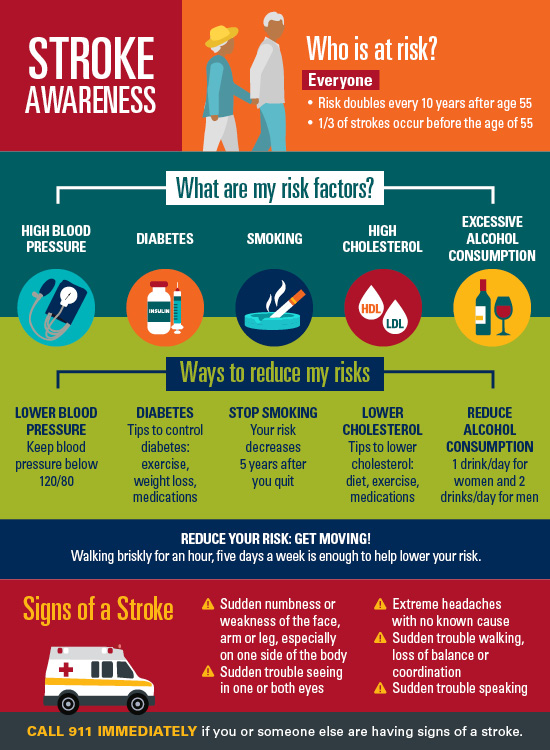
A stroke occurs when a vessel supplying blood to part of the brain is suddenly blocked, killing brain tissue. When you suspect a stroke, immediately call 911. Faster treatment means better long-term outcomes.
Recognizing the symptoms of stroke is key:
-
Sudden numbness or weakness of the face, arm or leg
-
Sudden trouble seeing
-
Sudden trouble speaking
-
Extreme headache out of nowhere
-
Sudden loss of balance or trouble walking
Immediate treatment is focused on restoring blood flow. Treatment may involve the use of clot-busting medications or a procedure to physically remove the blockage.
How strokes happen
Once someone is stable, our focus turns to rehabilitation preventing additional strokes. Often, a patient’s first question is, “Why did this happen?” Finding the stroke cause is crucial to determine the risk of recurrence and the best prevention.
So, why did the vessel become blocked in the first place?
Four common stroke causes:
-
Large-artery problems: Plaque buildup and narrowing of the large arteries in the head and neck. This is usually due to high blood pressure, high cholesterol, diabetes or other risk factors.
-
Small-vessel problems: Damage to smaller blood vessels deep in the brain. This is also usually due to risk factors such as high blood pressure, high cholesterol or diabetes.
-
Cardiac source: Clots from the heart travel to and block vessels in the brain, causing stroke. Most commonly a heart rhythm problem (atrial fibrillation) but potentially due to other heart conditions such as heart failure or heart valve problems
-
Stroke of other determined cause: Less common but well recognized causes such as vasculitis (vessel inflammation), dissection (physical tear in a vessel) or clotting disorders.
How stroke is diagnosed
The initial workup for stroke is aimed at identifying the most likely reason for a blocked vessel. First, we look at the vessels (CT or MRI) to check for major narrowing. We also check for stroke risk factors (high blood pressure, cholesterol, diabetes) and assess the heart for structural problems or abnormal rhythms.
After this initial workup, up to 30% of strokes do not fit neatly into one of the four categories above. Strokes without a known cause are called “cryptogenic” strokes.
Types of cryptogenic strokes
Not knowing the cause of a stroke can be extremely frustrating. In cases of cryptogenic stroke, an even more detailed workup is required.
Cryptogenic strokes may be caused by:
- Atrial fibrillation or afib
- Patent foramen ovale (PFO)
- Clotting disorders
- Aortic arch atheroma
Other rare causes of cryptogenic stroke include cancer, heart valve disease and other types of heart disease.
Atrial fibrillation (Afib)
Atrial fibrillation (Afib) is an irregular and often very fast heart rhythm. Afib occurs when the upper chambers of the heart beat irregularly. This causes blood to pump inefficiently, and clots can form within the left atria. A blood clot can then travel out of the heart to the brain and cause a stroke.
Symptoms of Afib can include
- Heart palpitations (hard, fast or irregular heartbeats)
- Lack of energy/fatigue
- Shortness of breath
However, some patients have no symptoms, making detection difficult. To complicate matters further, patients may only have Afib for a short time, followed by normal heart rhythm. One snapshot in time might not tell the whole story.
In these cases, prolonged heart monitoring may be useful. Some monitoring devices can be placed under the skin on the chest and monitor the heart rhythm 24 hours a day. If the device detects atrial fibrillation, patients are notified immediately. Your doctor may then suggest stronger blood-thinning medicine to prevent strokes. Some implanted heart monitors can be left in place for up to three years.
Patent foramen ovale (PFO)
Patent foramen ovale (PFO) is a small opening between the two upper heart chambers that never closed after birth. About 25% of adults have a PFO. Most people with a PFO are completely asymptomatic and never require any type of treatment.
In rare cases, however, a PFO may allow a blood clot to travel to the brain, causing a stroke. Although rare, this is possible in younger people without another explanation for a stroke.
Depending on age and other factors, your doctor may close the PFO to prevent additional strokes. PFO closure is a minimally invasive procedure performed through a small catheter inserted into a leg vein.
Clotting disorders
A clotting disorder is a condition where a person’s blood has an increased tendency to form clots. There are many different types of clotting disorders. Some are inherited and others are acquired later in life without a family history. If a person tends to form clots, those clots can travel to the brain and cause stroke. Depending on age and family history, additional labs may identify the underlying clotting disorder.
Aortic arch atheroma
An aortic arch atheroma is a build of plaque within the aorta, the largest artery in the body. The specific part of the aorta that comes off the heart is called the aortic arch. When plaque builds up within the aortic arch, pieces can break off and travel downstream, potentially blocking vessels in the brain and causing a stroke. The same risk factors for plaque buildup in the carotid arteries apply to risk of plaque formation in the aorta.
Treating strokes where the cause is unknown
If you or a loved one has had a stroke, talk to your doctor about the potential causes. Your doctor can perform additional workups to get to the underlying issue. Regardless of the cause, it is also important to address any other contributing factors such as high blood pressure, cholesterol, diabetes and tobacco use. By knowing these potential causes of stroke, working with your doctor can dramatically reduce the risk of having another stroke.



