Everything you need to know about colon polyps: Symptoms, causes and types
A colon polyp is a small growth in the lining of the colon or large intestine. Most colon polyps are sporadic and occur randomly. However, there are environmental and hereditary factors that increase the risk of developing colon polyps.
The most easily identified risk factor for developing colon polyps is age. That’s why we recommend colon cancer screening starting at age 45.
What genetic factors increase the risk of developing colon polyps?
You have a higher risk of developing colon polyps if you have a family history of colon polyps. There are also genetic syndromes that may increase your chance of developing polyps or of having these polyps transform rapidly into cancer.
Examples of genetic syndromes include:
Familial adenomatous polyposis: FAP is a rare, inherited condition that causes the development of polyps in the gastrointestinal tract.
Lynch syndrome: People with this condition can develop colon polyps. Although a small number of polyps typically develop, they have a higher risk of becoming cancer compared to polyps in the general population.
“All of these factors are considered by your doctor when recommending colorectal cancer screening,” says gastroenterologist Suha Jabak, MD. “If you have a family history of colon cancer or a familial syndrome of polyps, you should begin screenings at a younger age and have a more intensive surveillance protocol.”
Environmental factors that can increase your risk of developing colon polyps
While you can’t stop growing older, you can make lifestyle changes that can decrease your risk of developing colon polyps. These modifiable risk factors include:
Smoking
Excessive alcohol intake
Obesity
Lack of physical activity
Eating a lot of red meat or having a high fat/low fiber diet
What symptoms indicate colon polyps?
“Unfortunately, colon polyps usually don't cause any symptoms,” says Dr. Jabak. “Without any symptoms, polyps can develop and get bigger without you knowing. That's why we recommend screening.”
In rare cases, polyps can ulcerate and cause symptoms such as bleeding. In those cases, you may notice bleeding from the rectum. Some polyps can bleed microscopically, causing iron deficiency anemia. For that reason, if a male or a postmenopausal female develops iron deficiency anemia, their doctor may recommend an endoscopic evaluation for polyps.
How are colon polyps diagnosed and treated?
If you’re at average risk, your doctor will recommend screening using a stool test or colonoscopy at the age of 45. For those at higher risk of developing colon cancer, doctors will recommend starting screening at an earlier age.
“Stool tests do relatively well compared to colonoscopies in detecting cancer,” says Dr. Jabak. “However, stool tests have a lower sensitivity for detecting polyps, especially the smaller ones. For smaller polyps, colonoscopy is a more accurate diagnosis because a doctor is using a camera to detect the polyps visually.”
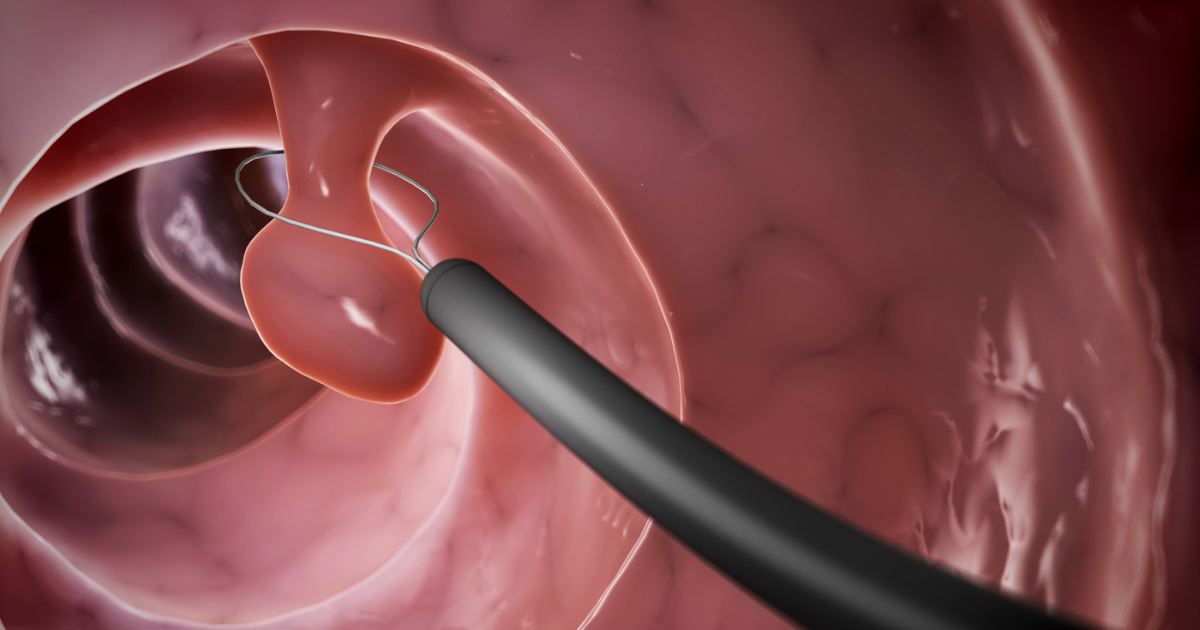
If a stool test is positive, you’ll need to have a follow-up colonoscopy. The benefit of a colonoscopy is that your doctor can remove any polyp they find during the procedure. This is usually done using simple techniques such as a snare to cut off the polyp.
“There have been many advances in this field, not only in the techniques used to remove polyps but also in diagnosis and imaging of polyps,” says Dr. Jabak. “Now, we use different imaging tools and dyes to determine, during the colonoscopy, whether a polyp has the potential to progress into cancer or whether cancer is already present.”
Advances in technology have also allowed us to remove large polyps and polyps with early cancer endoscopically. All polyps will be sent to pathology to be examined under a microscope to confirm the diagnosis.
Types of colon polyps
“We classify polyps as either benign or as having the potential to progress and develop into cancer,” says Dr. Jabak. “Not all polyps turn into cancer. Pre-cancerous polyps have the potential to turn into cancer if given enough time to grow,”
Pre-cancerous polyps typically take a long time before they progress into cancer. That's why colonoscopies are recommended. It allows doctors to detect and remove polyps before they become cancerous.
You should have follow-up colonoscopies after your initial colonoscopy. The timing for surveillance depends on the type, the number and the size of polyps found. If you have a larger polyp, one with more advanced histology, or have many polyps on your index colonoscopy, earlier surveillance is needed because of the higher risk of developing more polyps of the same type.
If you're over the age of 45 and haven't started colorectal cancer screening, have a family history of colorectal cancer or polyps, or have any symptoms that could suggest a cancer, discuss these with your doctor. To schedule a colonoscopy, call 800.922.0000.





