Strokes, seizures, brain fog and other neurological effects of COVID-19
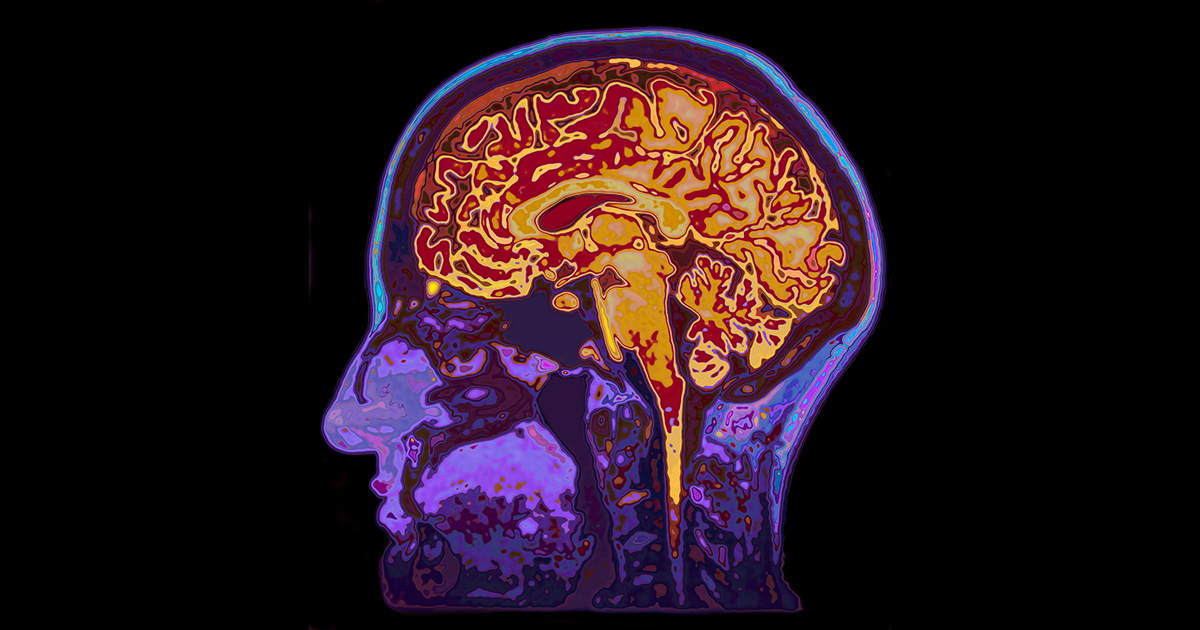
The brain is a complicated organ to understand in the best of times. And then you layer on the effects of a new – and constantly changing – transmissible virus. What neurologists are seeing in clinics and hospitals, however, is cause for concern.
"Brain dysfunction after COVID-19 infection is quite common," says neurologist Thomas Scott Diesing, MD. "Depending on how it's defined, between 40% and 80% of symptomatic COVID-19 patients have a neurologic complication."
But brain dysfunction covers a wide range of issues. "Brain dysfunction can be temporary, like delirium, which is very common in hospitalized COVID-19 patients," Dr. Diesing explains. "Or it can be permanent – from direct inflammation in the brain, to hemorrhaging and seizures."

"Permanent brain damage is more often a result of what the virus is doing in general to the body, like a blood clot that causes a stroke. Or the inability to form clots, which causes a hemorrhage and provokes a seizure. But it's rare to have a direct infection of the brain itself."
Who is more likely to experience brain dysfunction?
"I liken the neurological complications of COVID-19 to a tornado," says Dr. Diesing. "You know what a tornado is. You can prepare for it as much as you possibly can. But no matter how much you prepare, you're never really ready if it strikes you."
"The path is also unpredictable. Like a tornado, COVID-19 can affect one person quite severely and another person not at all."
People with certain medical conditions usually have a rougher time with COVID-19. They're more likely to develop any complication, including neurological.
How COVID-19 affects the brain
"The main symptoms you get from COVID-19 tend to be pulmonary, like cough or difficulty breathing," says Dr. Diesing. "But the virus can attack and infect any cell. The same receptors that the virus uses to get into lung cells are on brain cells and muscle cells and the cells in your sinuses. It just so happens that the pulmonary symptoms tend to be the most overwhelming."
Disproportionally, people with prior strokes and dementia tend to fare worse with COVID-19 than others.
Critically ill COVID-19 patients must be intubated or sedated. That can affect brain function.
Strokes after COVID-19
An increased risk of stroke follows COVID-19 infection. That includes asymptomatic people who contracted the virus. "COVID-19 causes blood clots in the legs, arms and lungs," says Dr. Diesing. "It's no surprise that people experience blood clots in the vessels going up to their brain as well."
"We've seen people without traditional vascular risk factors, who may be younger than normal, come in with a massive stroke," explains Dr. Diesing. "We're still working out the mechanism for why that happens."
But people with a higher risk for stroke – people with diabetes, obesity or who smoke – are more likely to suffer strokes after contracting COVID-19.
The good news: highly effective therapies can reverse the stroke or improve the outcome. Nebraska Medical Center is the only hospital in the region that's certified as a Comprehensive Stroke Center. If you or someone else has any of these symptoms, call 911 immediately or go directly to the nearest emergency room:
- Sudden numbness or weakness of the face, arm or leg, especially on one side of the body
- Sudden confusion, trouble speaking or understanding
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden, severe headache with no known cause
You can also remember the acronym FAST:
- Facial asymmetry
- Arm weakness
- Speech difficulties
- Time is brain
Long-term neurological effects of COVID-19
When new or recurring COVID-19 symptoms continue for weeks, you might be suffering from post-COVID syndrome (also called long COVID).
"Many COVID-19 patients recover from the acute infection, yet still are experiencing symptoms many months later," says Dr. Diesing. "Researchers and doctors are investigating why this is. It may be lingering effects of the virus, or from the body's recovery from the virus or something else entirely."
"Long COVID symptoms can include inattention, cognitive troubles, fatigue, behavioral troubles and other neurological symptoms," says Dr. Diesing. Brain fog (or trouble concentrating) is a common long COVID symptom, and may persist for weeks. Anxiety or depression can also follow a COVID-19 infection.
There's also the loss of taste and smell, which can happen during infection, and then persist as part of long COVID. "About 83% of people who have disorders of taste and smell will recover," says Dr. Diesing. "The average time to recover taste and smell is about 37 days. But there's a significant number of people who haven't recovered yet."
COVID-19 vaccines pros and cons
"The most effective treatment we currently have is prevention with COVID-19 vaccines," says Dr. Diesing. "The risk of neurological complications after vaccination is exceedingly small – especially compared to the neurological risks of COVID-19 infection. It's multiple orders of magnitude difference."
Blood clots in the brain, abdomen and legs, along with low levels of platelets – the blood cells that help you stop bleeding – have occurred in a small number of people who have received the Johnson & Johnson COVID-19 vaccine. The condition is called thrombosis with thrombocytopenia syndrome (TTS).
Symptoms begin approximately one to two weeks following vaccination. Most people who developed these problems were female, ages 18 to 49. This outcome is very rare. For women, the risk of TTS after J&J is four per million. For men, the risk of TTS after J&J is less than one per million.
Compare the neurological complications of COVID-19 directly to vaccination:
- Risk of neurological complications from COVID-19: between 40% and 80% of people who have symptomatic COVID-19. This means at least 400,000 per million people with symptomatic COVID-19 experience neurological issues
- Risk of TTS from vaccination: two per million people who receive the Johnson & Johnson vaccine. This means 0.0002% of people who get vaccinated with J&J experience TTS
Three safe vaccines prevent severe disease and death from COVID-19. Get vaccinated.




