How severe COVID-19 is causing unusual clots
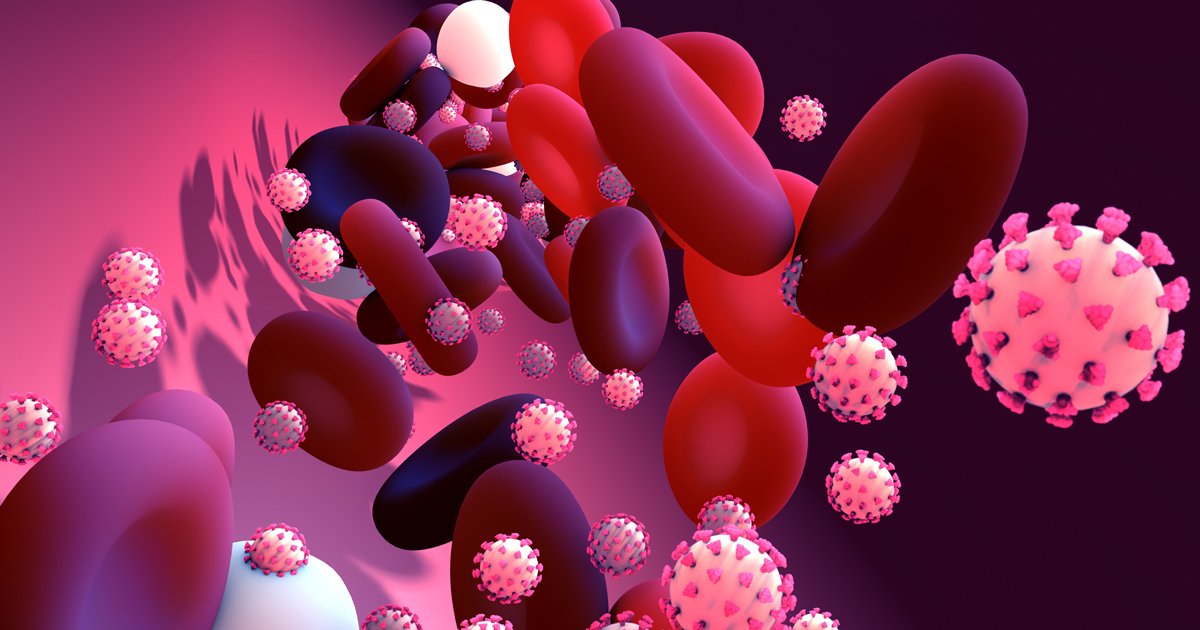
In addition to being a respiratory disease, COVID-19 is also affecting the circulatory system in some strange ways.
"In people with mild COVID-19 disease, it doesn't appear that their risk of clotting is higher than the average person. So we are not recommending COVID-19 positive people go on blood thinners or get screenings for blood clots," says vascular surgeon Matthew Longo, MD. But people with severe COVID-19 – those who are admitted to the ICU or put on a ventilator – are having more blood clots than the average person.
"Where we've seen a lot of trouble with COVID-19 blood clots is in veins of the legs and also in the lungs," says Dr. Longo.
How the virus causes clots: Infection, inflammation and injury
How are these more frequent blood clots happening? It appears that the coronavirus is getting into the wall of the blood vessel and causing infection of the blood vessel wall and injury. Once that happens, the blood vessel wall constricts and the factors causing clots to form are activated at the site of the blood vessel injury. The platelets start to collect at the site of injury and the clot starts to form.
Normally, the inside lining of a blood vessel wall releases a bunch of substances that prevent clots from forming. When the wall is infected and inflamed, it doesn't do that very well. In the critically ill patient, they are often experiencing a hyper-inflammatory response – which means the body's natural defenses are overreacting to the virus. "When people are in a hyper-inflammatory state, they naturally will make clots more often," says Dr. Longo.
One part of the body that is particularly affected are the lungs. Neutrophils, which are part of your immune system, can create webs or traps which normally contain infections. However, when coupled with increased activation of the clotting factors, a patient can have an increase inflammation and blood clots in the small and microscopic vessels of the lungs.
Think of the neutrophils acting as your body's very own Spider-Man: they create web-like structures. When they're doing their job during an infection, the neutrophil's web traps capture invaders. But if the neutrophils shoot too much webbing, it's not great for your body. And in the case of COVID-19, it can increase the risk of clots in your lungs, where there's supposed to be air instead.
"This is one of the major reasons why people can't breathe and have to be put on a ventilator," says Dr. Longo. "Normally, where you'd exchange oxygen in the lungs would be in these microscopic blood vessels. But if the blood vessels are filled up with clot, there isn't the ability of oxygen to go from the lungs into the body. So they can't breathe."
How COVID-19 affects the circulatory system
Here are three unusual ways that COVID-19 is interacting with the circulatory system.
COVID-19 patients under the age of 50 have much higher rates of stroke than people their age without COVID-19.
The long-term circulatory effects of COVID-19 aren't known yet, but "they will depend on the co-morbidities of the patient and how severe their case of COVID-19 was," says Dr. Longo.
Finally, treating a clot for a COVID-19 patient is unusually difficult. Some people can clot even while on blood thinners, which is very strange. "The normal things we do to get rid of clots – dripping in a clot-busting medication or pulling the clot out in surgery – don't work, because the clot reforms right away," says Dr. Longo. In severe situations, people with COVID-19 sometimes need a foot or toe amputation to remove the clot.
More research is needed on why these things happen, since COVID-19 is still a relatively new disease. One of those researchers includes Paul Dobesh, PharmD, who just published a paper about COVID-19 thrombosis.




