What is sickle cell disease, and how does it affect the body?
Sickle cell disease, or SCD, is a group of hereditary blood disorders that affects the shape and function of red blood cells. While SCD impacts various aspects of a person's health and well-being, people with the condition can live full and rewarding lives.
Understanding sickle cell disease
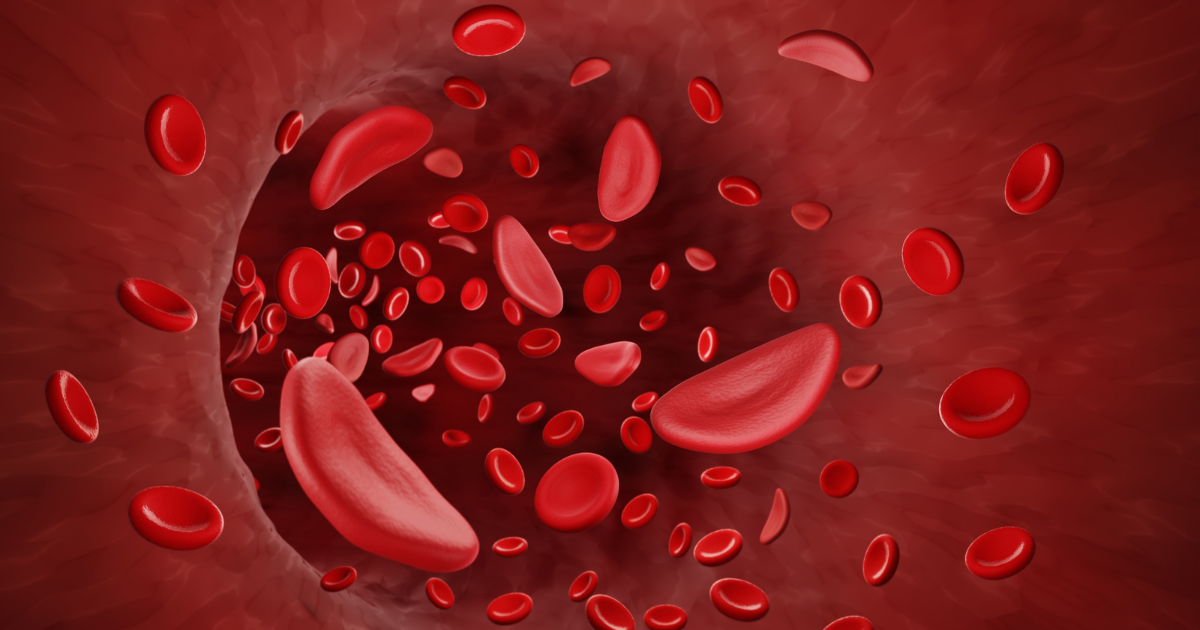
Sickle cell disease is caused by a mutation in the gene responsible for producing hemoglobin, the protein that carries oxygen in the blood. This mutation produces abnormal hemoglobin, which causes the red blood cells to become hard and sticky. The sickle cells die early, resulting in anemia.
“Not only do the blood cells get stuck and block up the blood vessels, but they also break down and don't last as long,” explains hematologist and oncologist Alex Nester, MD. “And that, unfortunately, can affect almost every part of the body, from your eyes down to your skin and your toes.”
Symptoms
The symptoms of SCD can vary in severity and may include:
- Anemia. This occurs when there is a shortage of healthy red blood cells, leading to fatigue, weakness and shortness of breath.
- Pain crisis. Also known as a vaso-occlusive episodes, a pain crisis occurs when sickle cells block blood flow, causing severe pain in the affected area.
- Strokes. A lesson common symptom, strokes can occur when sickle cells block blood vessels in the brain.
- Acute chest syndrome. Less common is this is condition, characterized by chest pain, fever and difficulty breathing.
How is sickle cell disease diagnosed?
Sickle cell disease is screened for at birth through a simple blood test. This screening helps to identify infants with the condition early on, allowing for early intervention and management.
Treatment options
Treatment options for SCD aim to manage symptoms and prevent complications.
- Blood transfusions. These may be used to increase the number of healthy red blood cells and improve oxygen delivery.
- Medications. A common medication, hydroxyurea, can stimulate the production of fetal hemoglobin, which helps prevent the formation of sickle cells. Recently, two novel medications, crizanlizumab and veloxetor, have been approved for treating SCD, offering new hope for patients.
- Gene therapy. This approach involves modifying the patient's cells to produce normal hemoglobin and prevent the formation of sickle cells. In December 2023, the Food and Drug Administration approved the first cell-based therapies for the treatment of SCD in patients 12 years and older.
Quality of life
The impact of SCD on a person's quality of life depends on the severity of the disease. Some individuals may experience minor symptoms that come and go, while others may have significant and chronic pain. Long-term complications can include liver disease, blood clots, kidney damage, eye problems, lung damage and pulmonary disease.
Lifestyle behavior modifications can help reduce the occurrence of pain crises. These include:
- Drinking plenty of fluids to prevent dehydration.
- Avoiding extreme temperatures, both hot and cold, which can trigger pain crises.
- Avoiding high altitudes or situations that might produce low oxygen levels, such as extreme exercise and overexertion.
SCD patients need to stay updated with vaccinations, as they are more susceptible to infections. Blood donation is also crucial for those who may require blood transfusions. Lastly, getting on the bone marrow transplant registry can offer the potential for a cure for some patients.
Getting support
It can be helpful for SCD patients and their families to get involved in support groups or connect with others in the sickle cell community. These communities provide emotional support, information sharing and a sense of belonging.
“I find it can be very beneficial for sickle cell patients to see people who are thriving despite their disease, who may have their struggles and need a lot of medical care but still able to maintain a happy and successful life,” Dr. Nester says. He adds that SCD is not well understood by society at large, which can cause conflicts between patients and their employers, medical providers and others.
“They might not understand when someone suddenly calls in and says, ‘I'm so sorry, I can't move, I'm in terrible pain,’” he says. “And then they come back three days later and look quite well. It's a very common concern for sickle cell folks, and as a provider, I can only tell them I hear this from many people. Just knowing that there are other people out there that have had the same experiences really helps.”
As SCD is a lifelong condition, being seen regularly by a hematologist is important.







